Karen Calder (32), originally from Belfast but now living in Kilkeel, started getting pains in her neck at 19 years of age. Over time, this progressed into prolonged periods of generalised pain all over her body. Finally, after many years of attending her GP and asking for referrals to specialists, Karen was diagnosed with mild joint hypermobility and fibromyalgia in 2017.
While a diagnosis is a positive step in the treatment process, there is no known cure for fibromyalgia, and the medical profession are still unsure as to how it develops in the first place. This means around 24,000 individuals in Northern Ireland, including Karen, live with the invisible but very painful condition fibromyalgia and another 7,000 with M.E (Myalgic Encephalomyelitis) that directly impacts on their ability to live a normal and independent lifestyle.
“For someone who doesn’t have fibromyalgia – imagine having a bruise and continuously pressing it – it hurts. Imagine having that bruise covering your entire body. You can’t walk far without pain in your legs, you can’t brush your hair without pain in your scalp. You can’t get anyone to listen to you when you try to explain your symptoms, so it’s like yelling at the top of your lungs with no sound coming out. It’s incredibly frustrating” explained Karen.

Receiving a diagnosis of fibromyalgia is often and long and complicated process, with many individuals having more than one condition affecting them. Karen received her diagnosis in 2017 after a long process of trying to identify what was causing her pain.
She said: “Fibromyalgia makes many simple, daily tasks a struggle for me – I can’t clean my house or change my bed, and I struggle to have a shower or wash my hair on my own. I worked from the age of 16 but when the symptoms of my condition worsened, I became unemployed and haven’t been able to work since. I am currently trying to do a degree in health and social care.
“I had been getting pains in my neck for around ten years, and every doctor I went to said it was stress or tension. When the pains began to spread to other areas, friends thought it sounded like fibromyalgia. It was a very difficult time; I was in constant pain, but it felt like no one understood or believed just how bad it was. I fought with my doctor for about six months for a referral and finally got to see a rheumatologist. I was diagnosed with mild joint hyper mobility and fibromyalgia, and I had an MRI that showed wear and tear in my back and neck. I finally had proof that the pain I had been having for ten years or more wasn’t from stress.
“I had also been to numerous doctors because I had been having palpitations and I was told many times that it was anxiety. One night in 2014, the palpitations were so bad that I couldn’t move, so I phoned an ambulance. I was taken to hospital and kept in for five days before being diagnosed with supra ventricular tachycardia (SVT). In addition to fibromyalgia, I had been living with an undiagnosed heart condition.
“In 2015, I had an ablation and was told it was fixed, but it came back, so I had to have another ablation in 2016. During the operation the surgeon discovered that I had an accessory pathway. The SVT was fixed but now I need to take a heart tablet for the accessory pathway and a side effect of that is breathlessness.”
Fibromyalgia is often misdiagnosed as anxiety or depression and just like living with all other chronic, life changing illnesses patients can suffer secondary depression or anxiety as a result.
Due to the impact the condition has on an individual’s ability to live a normal life – because of constant physical pains, lethargy, and fatigue – individuals do often suffer from mental health conditions in addition to fibromyalgia. This could be in part due to the long average length of time it takes to receive a diagnosis, the lack of treatment options available to help manage the condition, and the sense of isolation that individuals feel due to a lack of awareness and support.
“Fibromyalgia has changed my life – I struggle to lead a ‘normal’ life” said Karen, adding: “My relationships with family and friends have been affected, especially my relationship with my two young nephews who don’t understand why I can’t play with them and why I’m not a fun aunt anymore. I need help to do daily tasks at home, but because I can’t get a referral from my GP for a social worker, I’m not eligible for home help. I was told by a doctor that I cannot attend pain management classes because of my anxiety. He said that if I take a panic attack in the class it will disrupt the others and it wouldn’t be fair on them – but what about me?
“The medical profession absolutely doesn’t know enough about fibromyalgia, and it feels like a lot of them just don’t want to. My doctor said he read a book on living with pain and suggested I buy it. Another doctor in the same practice just prescribed me co-codamol, which doesn’t even work as pain relief for fibro.”

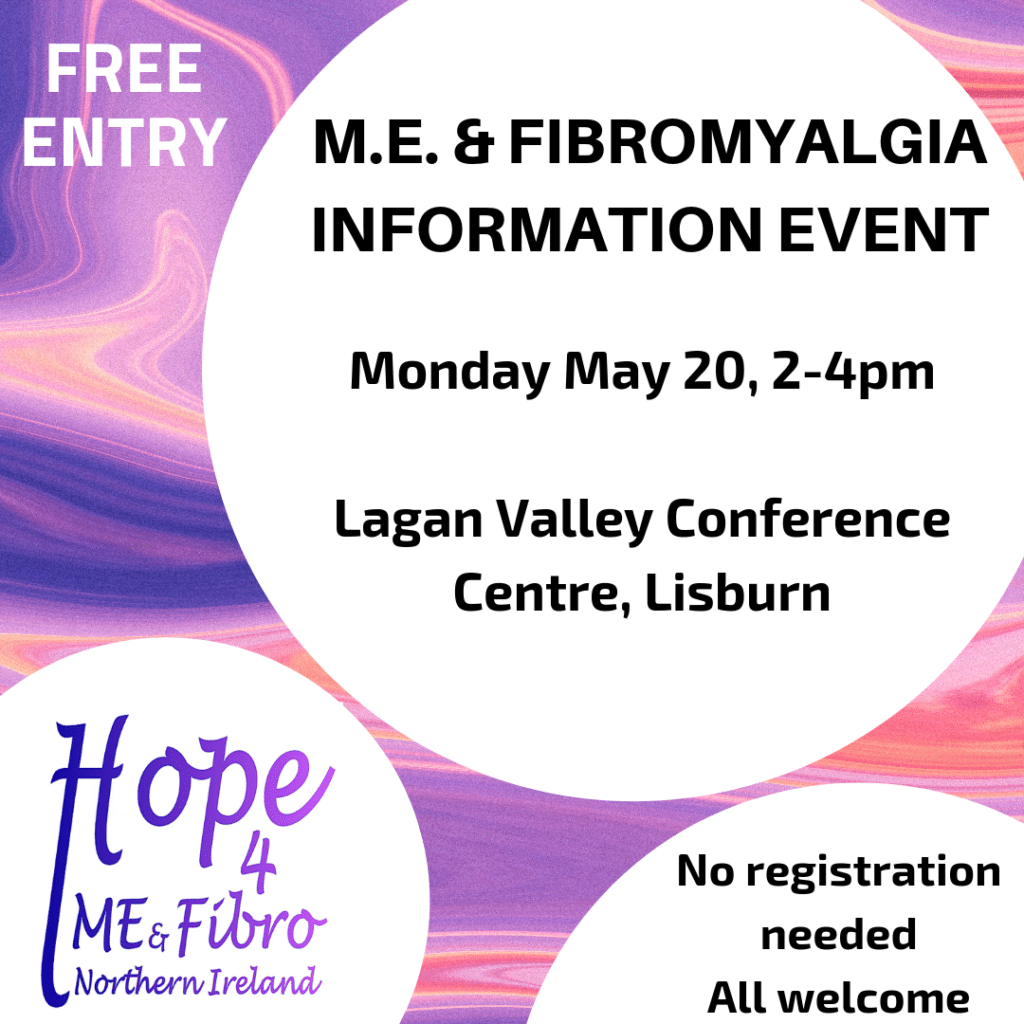
Local support organisation HOPE for ME and Fibro Northern Ireland is running a free event on Monday May 20 to help increase awareness about the conditions, with the aim of breaking the stigma surrounding the invisible but painful symptoms of fibromyalgia and M.E.
‘Stigma and ME & Fibromyalgia is Real’ is a free awareness and information seminar being held on Monday, 20th May in the Lagan Valley Conference Centre, Lisburn, for 2pm to 4pm. Attendees can register on arrival.
For more information go to www.facebook.com/Hope4MEFibro

